Insulin resistance is often referred to as one of the most common health disorders worldwide, yet many people remain unaware of its presence until it develops into more serious conditions like Type 2 Diabetes. Insulin, a vital hormone produced by the pancreas, plays a critical role in managing blood glucose levels and ensuring energy is delivered to the cells. However, when insulin’s effectiveness diminishes, the consequences ripple throughout the body, leading to a cascade of metabolic issues.
What is Insulin Resistance? #
Insulin resistance occurs when the cells in your body no longer respond effectively to insulin. Normally, insulin helps transport glucose from the bloodstream into cells to be used as energy. When resistance develops:
- The cells become “deaf” to insulin’s signal, requiring the pancreas to produce more insulin to achieve the same effect.
- Over time, the pancreas works harder and harder, secreting increasing amounts of insulin, until it can no longer keep blood glucose levels in check.
- This eventually leads to Type 2 Diabetes (T2D) if left untreated.
Think of it as a miscommunication: insulin is shouting louder, but the cells aren’t listening.
Why Insulin Levels Matter #
Most people focus solely on glucose levels when assessing metabolic health. However, normal glucose levels don’t always mean you’re in the clear:
- Your pancreas may be overproducing insulin to maintain normal glucose levels, which is an early sign of insulin resistance.
- Measuring insulin levels alongside glucose levels provides a clearer picture of your metabolic health.
Key Blood Markers for Insulin Resistance: #
- Fasting Insulin: Greater than 6 µU/mL
- Postprandial (PP) Insulin: Greater than 30 µU/mL
- HOMA2-IR: Greater than 2 (a measure of insulin resistance)
- Triglyceride-to-HDL Ratio (Tg/HDL): Greater than 2
If these markers fall outside the normal range, it’s a sign that insulin resistance may be present.
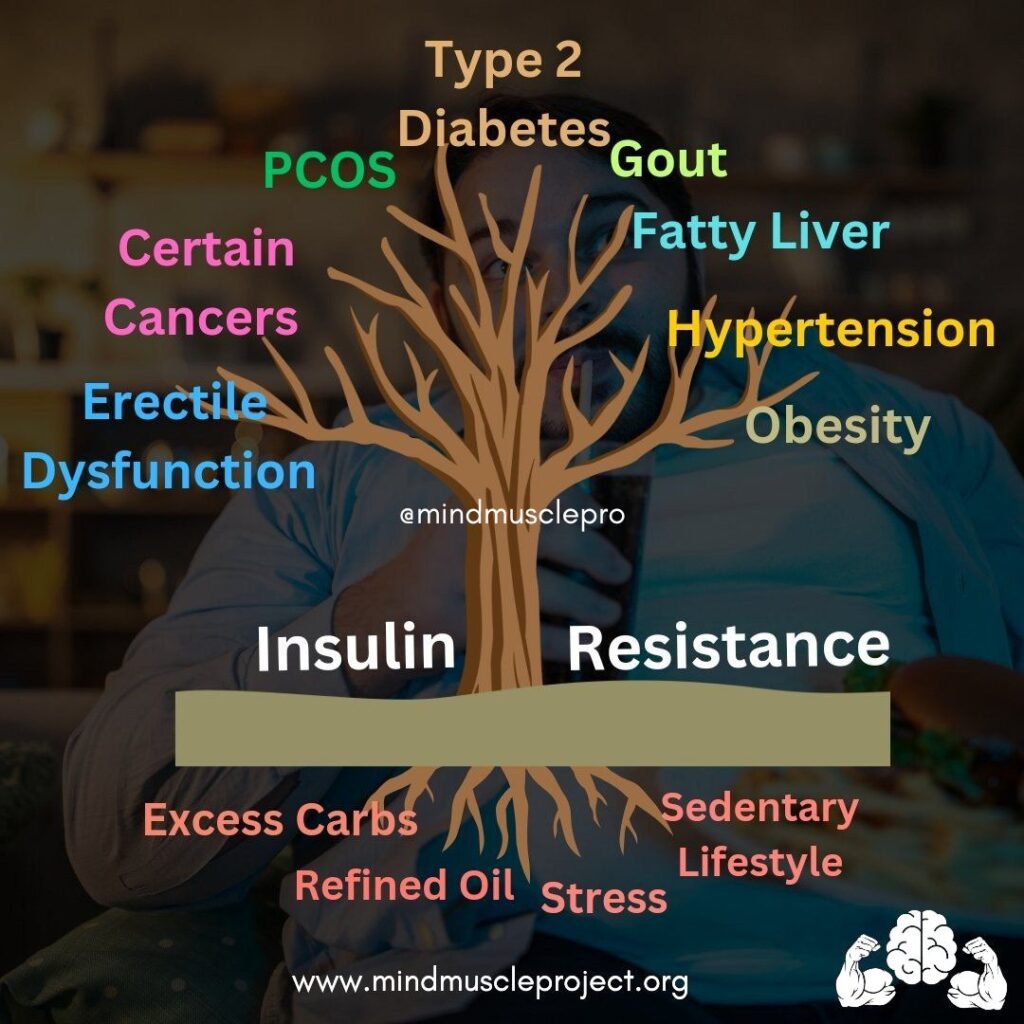
Causes of Insulin Resistance #
Several lifestyle and dietary factors contribute to the development of insulin resistance, including:
- Excessive Carbohydrate Consumption
- Carbohydrates, especially processed ones, cause the largest spikes in insulin. Over time, high carb intake strains the pancreas and leads to insulin resistance.
- Frequent Eating and Snacking
- Eating multiple times throughout the day keeps insulin levels elevated, reducing the body’s ability to regulate them effectively.
- Refined Oils
- Commonly found in processed foods, refined oils increase inflammation, worsening insulin resistance.
- Chronic Stress
- Stress elevates cortisol levels, which interferes with insulin’s function.
- Sedentary Lifestyle
- Lack of physical activity reduces the muscles’ ability to utilize glucose effectively.
- Nutrient Deficiencies
- Low levels of key nutrients like magnesium, chromium, Vitamin D, and zinc negatively impact insulin sensitivity.
Symptoms of Insulin Resistance #
Your body often provides early signs of insulin resistance, many of which appear on the skin. These symptoms may precede any noticeable changes in blood glucose levels:
Common Signs and Symptoms: #
- Skin Changes:
- Skin tags
- Darkened patches of skin on the neck or joints (Acanthosis Nigricans)
- Acne
- Weight and Fat Distribution:
- Increased belly fat
- Other Indicators:
- Sugar cravings
- Feeling fatigued after meals
- Excessive thirst
- Hirsutism (excess hair growth in women)
Conditions Linked to Insulin Resistance #
Insulin resistance doesn’t exist in isolation; it is often the precursor to a host of chronic health conditions:
- Type 2 Diabetes
- Non-Alcoholic Fatty Liver Disease (NAFLD)
- Polycystic Ovary Syndrome (PCOS)
- Obesity
- Hypertension (High Blood Pressure)
- Gout
How to Reverse Insulin Resistance #
The good news? Insulin resistance is reversible with lifestyle interventions and consistent effort. Here’s how:
1. Carbohydrate Restriction #
- Reduce your intake of processed carbs to minimize insulin spikes. Focus on whole, nutrient-dense foods that stabilize blood sugar.
2. Fasting #
- Implement intermittent fasting or time-restricted eating to lower the frequency of insulin spikes and improve insulin sensitivity.
3. Resistance Training #
- Exercise, especially strength training, improves glucose utilization by muscles and enhances insulin sensitivity.
4. Stress Management #
- Incorporate mindfulness practices, yoga, or other stress-reducing activities to keep cortisol levels in check.
5. Optimize Sleep #
- Prioritize 7-9 hours of quality sleep per night, as poor sleep contributes to insulin resistance.
Micronutrient Support #
Certain micronutrients play a crucial role in insulin sensitivity. Addressing deficiencies can provide additional support in reversing insulin resistance:
- Magnesium
- Chromium
- Vitamin D
- Zinc
- Cysteine
Final Thoughts #
Insulin resistance is a silent yet pervasive health issue that affects nearly every cell in the body. Left unchecked, it can lead to serious metabolic disorders, but the steps to address it are straightforward. By reducing carbohydrate intake, fasting, exercising, and addressing nutrient deficiencies, you can restore your body’s insulin sensitivity and reclaim your metabolic health.
Your skin, energy levels, and overall well-being will thank you. Take action today—small steps can lead to big changes in reversing insulin resistance and preventing chronic disease.